Best Practices for Tracking Temperature-Sensitive Medications in EMS

A surprising number of prehospital treatment protocols call for temperature-sensitive medications. Cardiac arrest, allergic reactions, pain control, sepsis response, whole blood deployment, and many other responses require medication that’s safely and carefully stored.
So, how do you keep track of that medication and make sure it stays within the temperature window at all times, especially in a hot ambulance compartment? Here’s what you need to know about tracking the medication cold chain to ensure your patients stay safe.
Why Temperature Tracking Matters in Prehospital Medicine
EMS providers respond in the real world. Unlike hospital pharmacies with controlled storage environments, EMS workers face extreme weather, long transport times, overnight truck staging, and fluctuating temperatures in engine bays (not to mention all the other variables that can factor into an emergency).
All of these aspects contribute to medication storage that’s rarely ideal. But every dose of medication you administer in the field must be at the highest standard of strength, quality, and purity as it had when it left the manufacturer. Breaking the cold chain means that medications degrade, lose potency, and separate. Temperature changes can also cause preservatives to break down.
Medication viability has a set time frame—a temperature window—where it is safe. There’s no room for error. A vial left in a hot compartment for a few hours can go from offering life-saving efficacy to compromised performance. What’s more, it can be hard to know when that window has been exceeded.
Even knowing that a medication has gone outside the cold chain is only half the battle. Once you know it’s been exposed, you’ll need to waste and discard the medication, which adds to inventory costs and limits your team's access.
A better approach is to carefully track the chain of custody throughout the entire life of the controlled substance. Careful tracking helps you anticipate common failure points and meet all recommended storage guidelines.
A medication that’s become ineffective due to temperature exposure is equivalent to no treatment at all. When medication degrades, it can also cause unpredictable results and even adverse reactions.
Wasted medication increases your spending in an environment that’s already highly budget-constrained. Should something go wrong with the medication, the cost can be even higher. Lost temperature data is essentially indefensible in quality reviews and litigation. Your tracking and documentation protect your team and your patients.
Understanding Temperature-Sensitive Drug Storage Requirements
Now, not all temperature-sensitive medications have the same guidelines and restrictions, and not all temperature-sensitive medications even require cold storage. Some medications require refrigeration (2–8°C / 36–46°F), while others may require controlled room temperatures (20–25°C / 68–77°F). Some medications can handle short windows within labeled ranges, and others are rendered immediately unusable.
Your EMS agency needs to have clear records of all manufacturer storage ranges for each medication. These records should be easy to access and known to all personnel who handle the drugs. Guidelines should indicate any allowable excursion windows by duration and temperature, as well as the shelf-life of the substance once it’s been moved out of refrigeration.
In the manufacturer’s information, you’ll find guidelines for beyond-use dating and post-warm use storage. You’ll also learn about light sensitivity and other handling notes. The guidelines should outline disposal rules and information for medication that’s been exposed beyond the limits.
While some of these manufacturers’ guidelines can seem like “pharmacy language,” it’s important that your crew knows all the rules. It’s part of operational direction, and it can help them make the right choice when they’re under pressure.
EMS agencies should have a secure and standardized medication policy that’s written with the realities of EMS in mind. Temperature logging procedures should be documented for all stations and units, and steps should be defined for the moments when excursions occur.
Clear labeling on kits, drug bags, and fridges is essential to the process. Drug storage guidelines must be simple, visible, and enforceable (not in a PDF in a drawer that no one reads).
Historically, many EMS agencies have relied on paper or manual tracking to keep a handle on temperature. While it might seem convenient in the moment, the truth is that there are many problems with paper tracking. Clipboards get wet, sticky notes get lost, and pens stop working. Every shift change introduces more variability.
Plus, a medic who’s running three back-to-back emergency calls doesn’t have the time to stop, find, decipher, and fill out a log sheet. Even if they care, reality can move too fast to keep up. Manual systems lead to inconsistent documentation, illegible entries, skipped temperature checks, and delayed data review to catch it all. Paper doesn’t alert you when medications drift out of range.
If your refrigeration system fails at 3 AM but doesn’t get noticed until 7 AM, everything in the system is likely compromised. Without digital tracking, your information is limited to whatever was written down, assuming it was written down at all—that’s too ambiguous for something so important.
Establishing a Strong EMS Cold Chain Workflow
Reliable medication management plans are built around predictable processes. There should be standard stopgap rules for the process. That means controlled storage at every step, continuous monitoring, and timestamped excursions. Med kits need to be treated like perishables, not like general equipment.
In an environment where everything is based on preparedness, it’s tempting to bring refrigerated meds to “ride along just in case.” But those meds that must travel need to be carefully stored in validated coolers and temperature-controlled environments for the entire duration.
When a medication is exposed to temperatures above the limit, it should be documented. The information needs to include what happened, how long it lasted, which range was exceeded, who handled it, and the final disposition (return to stock, discard, replace).
Inventory should be very carefully monitored. Restock first-expiring meds, then rotate inventory. Double-check the seals and verify temperatures before loading it into rigs. Digital tracking makes these jobs infinitely easier. It also increases compliance by creating built-in accountability. You catch mistakes before they happen, while they’re still preventable.
Environmental Challenges Unique to EMS
In EMS, temperature compliance is a significant challenge. The realities of field work don’t offer consistent temperatures or environments. Units might be staged outside in freezing conditions or face summer temperatures exceeding 120°F. If units are on standby or have long travel, storage must be prioritized and confirmed.
Then there are the unplanned factors like power loss during a storm. Even delays during transfer-of-care or in rural settings can take medication out of the safe zone if you don’t have flexible, mobile cold chain options like temperature-controlled bags, insulated containers, and data logging protocols to capture real-time stats.
We all know how it is to go into a shift with guesswork. No one should walk into their day wondering what happened to a medication before their shift. Clarity saves time, and that time can help you save lives.
Additionally, the truth is that medication loss is very expensive, especially when it comes to high-value drugs and refrigerated products that have a limited shelf life. Without the right tracking, your agency may discard meds as a safety precaution, when it’s really preventable waste.
By documenting meds properly, you’ll reduce unverified discarding due to missed documentation. You’ll rotate inventory more efficiently and be more aware of storage locations and processes that are prone to temperature drift.
Documentation also helps you forecast your purchasing needs by allowing you to compare actual usage data to inform your decisions. The result goes beyond safer meds and gives you more budgetary control and better readiness for calls.
What Good Temperature-Sensitive Med Tracking Looks Like
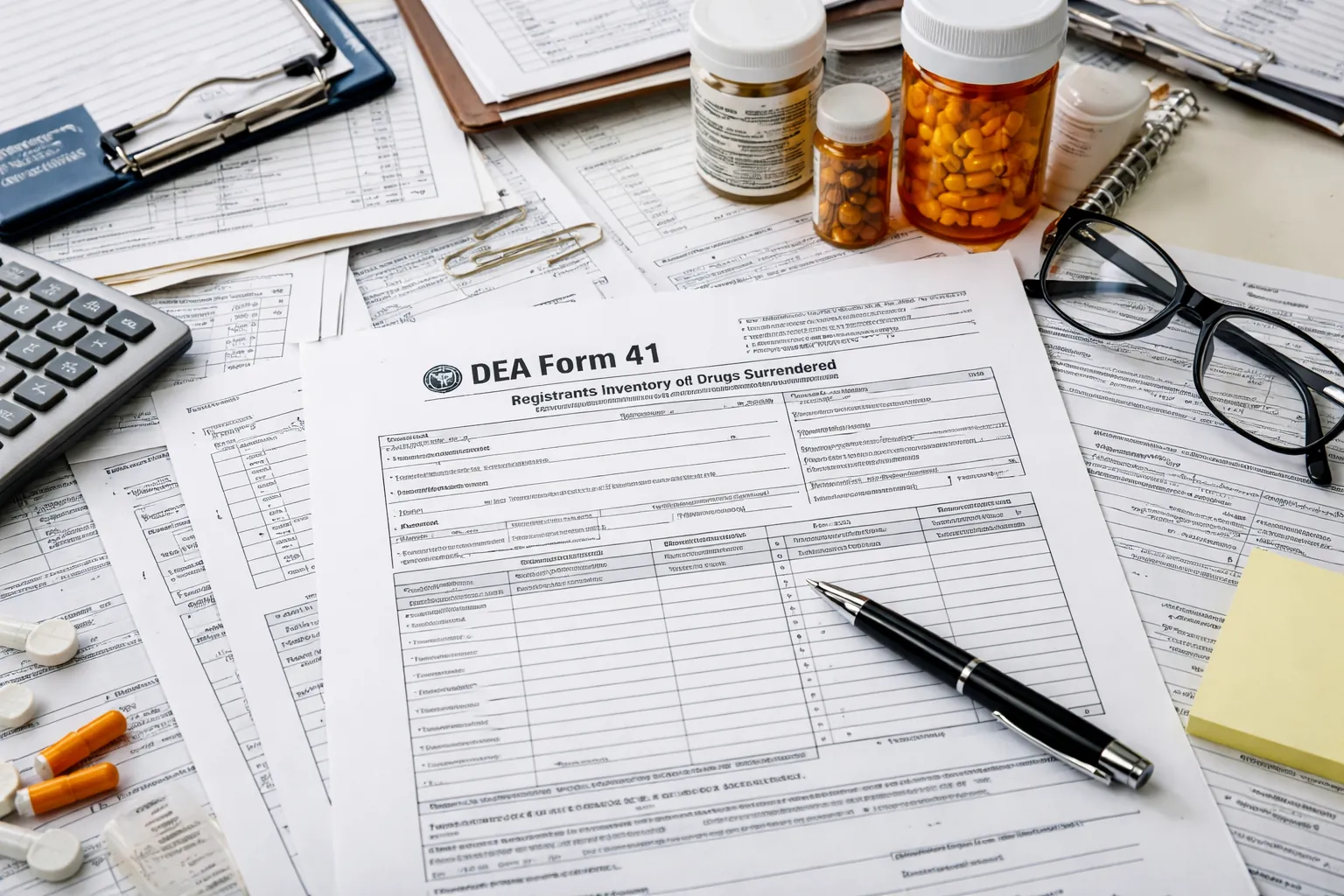
So, what does good documentation look like? While the exact standards and protocols will vary by organization, state, and federal guidelines, there are universal standards for quality tracking.
In an audit, it’s not about what you think happened; it’s about showing the proof. Strong documentation backs you up with clear temperature tracking and chain of custody visibility. Tracking can be drilled down to the lot numbers and expiration dates of each vial kit or box, so it’s easy to identify any anomalies.
Another strength of having a tracking system is that you’re aware and alert when something goes out of range or when inventory is running low. With LogRx, you can check replacement notifications for shortages and expirations to make sure your crew is never without the medications they need.
Digital tracking has become the standard in EMS, though many agencies still rely on manual logs. Digital medication management platforms like LogRx make it easy to transition to an improved system.
With LogRx, you get barcoded medication tracking and mobile app access for field crews, right from their handheld device. With a quick scan, they can document where and when the medication is being used, and the path of any vial can easily be retraced.
LogRx also offers real-time temperature monitoring. We pair our tracking module with a wireless temperature sensor. That means any time your meds drift out of the safe temperature zone, your crew will get notice.
While our temperature monitoring technology is in beta testing right now, we will be opening it up to all users in the near future. The temperature tracking feature will integrate with existing LogRx modules, so you can be in the know, no matter where you are.
For administrators, LogRx keeps you audit-ready and risks that can arise from gaps in tracking. There’s no recreating the past; you’ll have historical audit trails to help you keep a handle on everything right from the administrative dashboard.
Higher-accuracy tracking is particularly valuable for temperature-sensitive medications such as epinephrine, calcium, and insulin, as well as other treatments that can degrade rapidly with temperature fluctuations. With a digitized process, you streamline and simplify a job that could take hours or days to organize on paper.
Protecting your EMS cold chain requires visibility and accountability. When your documentation stands up to scrutiny, your waste decreases, your audit stress is lowered, and crews feel protected. Most importantly, patients receive the true therapeutic treatments that they need in emergencies.
If you’re ready to move your crew forward with accurate, user-friendly medication tracking, reach out to LogRx today. We’re happy to demonstrate how proper tracking can be a game-changer for your organization.




















.webp?t=1771620461097)